If you’ve come across this blog before you’ll have noted a few things.
As an Irishman, an Irish doctor with broad interests, I’ve been reading and writing quite a bit about stuff called Economics lately.
Now Economics sounds dry and dull, but the more good books I’ve read on the subject, the more obvious it is that understanding it is key to lots of stuff.
We certainly know that understanding economics is important to us, as the risks posed by Brexit and Trumpit are significant threats to Ireland’s future,… we need to box clever at this time.
So I’m going to add a further post here to 2 earlier posts about Ireland , #1 about Ireland’s #1 crisis which is housing, #2 about Ireland’s healthcare challenge to come to #3
It’s 2017, Ireland needs to improve its healthcare system – its time to take an innovative path forward with better #HealthIT.
So here we are looking at Ireland/ its healthcare system/ its need to get digital in the 21st Century and the related need to innovate our way there.
(NB If you’ve come to this blog in the past you will know that the move to bring healthcare into the information age is now the main focus of my work hence topic#3.)
We mentioned the Irish healthcare system needing reform in our last post and the potential of the SlainteCare plan therein.
We know the SlainteCare report called for a transition & legacy fund of £3 billion of investment over the next 6 years as part of a 10 year reform programme.
We also know the Budget of recent weeks failed to find the funds to kickstart that programme, just yet.
On the issue of moving the Irish health service into the information age, we know that large parts of it have years/decade of catching up to do.
We know that eHealth Ireland’s related plan to seek €875m over 10 years to fund a related Electronic Health Record programme has been in waiting for some time now.
We also know that ask for €875m made that it into the SlainteCare report and for better/worse the funding request could/may be linked within the SlainteCare programme.
We also know there are real and substantial risks when planing to spend that sum of money on healthIT, billions were wasted elsewhere, so we can learn from this.
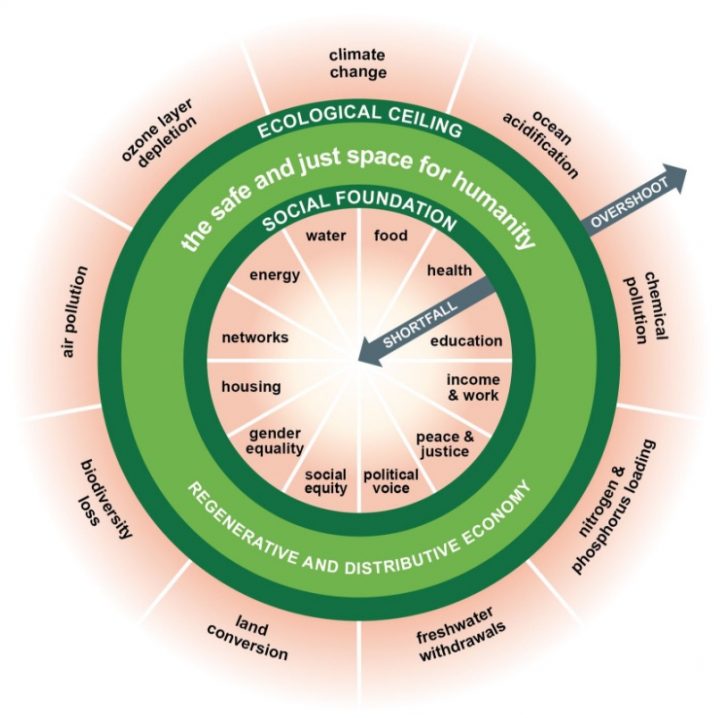
So lets tease out some of the key issues on Ireland’s move to digitise healthcare, again re-exploring the key aspects via the approach taken in “7 Ways to Think like a 21st Economist“.
The key (bottom line TL;DR) points are
The State which is essential- so make it accountable – needs to educate and build capacity/capability & be v careful what it procures
The Market, which is powerful , so embed it wisely – we need to move the market towards user centred digital services based on an open platform in healthcare
The Household, which is core, so value its contribution – the patient should be at the centre of healthcare – so build a patient centric platform
The Commons, which are creative, so unleash their potential – so nurture an open digital commons in healthcare to transform

The State which is essential- so make it accountable
So lets start by looking at the role of the State in this move to digitise healthcare.
Its been clear for years that the Irish healthcare system has not yet made the move towards a digital health service in most areas of practice. Aside from Primary Care/GPs where there is a high level of computerisation, the majority of community, hospital, mental health and social care is supported with paper records. Simply put Irish healthcare is still in the information dark ages.
We know there has been report after report over many years to try to move that agenda on, yet the legacy of PPARS cast a long shadow and so there was very little innovation in healthIT for a long time here. That began to change when eHealth Ireland was set up in 2015 and the team involved have worked hard and done some good stuff. Where things have gotten stuck of late is in move towards the adoption and rollout of Electronic Health Records (EHR).
Now I’ve been on the record for some time, to suggest caution when tackling Electronic Health Records projects/programmes as I guess its probably fair to say this is now my particular area of expertise, based on over 15 years in the field of informatics at departmental/hospital/city/regional/national/international levels. You may be interested in some key suggestions made as part of the eHealth Ireland public consultation on EHRs, early in 2016.
- Clinical leaders need support and guidance on the road towards 21st Healthcare
- Agile and Iterative Improvement towards integrated patient care is key
- Open Platform Technology allows for greater integration, collaboration, flexibility and reuse
- Investment is required but should be spent wisely…billions were wasted elsewhere, we can learn from this.
- Any other path risks perpetuating the current disconnects and related pressures.
Nevertheless, sometime later last year eHealth Ireland appeared to be moving down the traditional “big procurement” approach to buying EHRs, i.e.
€875m spend on EHR over 10 years made up of 4 key parts ; an acute EPR; a community EPR; an integration platform; and a national shared record provided via a portal
Now we know from experience (including some of my own) in large national eHealth/EHRs pushes in the NHS and the US that there has been billions wasted on EHRs before.
At that time and since that time, indeed for too long, I have seen “poor customers” make poor decisions in this space on behalf of the taxpayer, on behalf of the state.My own experience and looking at the leaders in this field internationally, one needs a small/highly educated/experienced group across clinical/managerial/technical disciplines to make good decisions on EHR decisions and the norm is to make mediocre decisions, i.e. I’ve seen many teams make naieve mistakes and then admit sometime later they have learnt some of these lessons the hard way..
To explain further why I start here, it is important to acknowledge the relatively immature state of informatics as a discipline in healthcare. Up until this year there was no recognised training body in the UK for Clinical Informatics . In fact the Faculty of Clinical Informatics in the UK has just appointed its very first Founding Fellows in recent months, which gives you some idea of the level of digital literacy in the medical profession at this point in time. The NHS Digital Academy has been announced, but has yet to get started. To reinforce the same point locally, there is simply no formal training or recognition of the science/art of clinical informatics in the Republic of Ireland. None.
So there is a major educational gap in the professions and indeed across our universities and so a real need to ensure staff have the right level of understanding of the complex people + process + technical aspects that are involved in digitising healthcare. Simply put Ireland has a very limited informatics capacity at this point in time.
In the context of that environment, where experience with EPRs is very limited in Ireland, then any EPR/EHR project is by nature going to be risky here, so the key is to start small and be agile and iterative in the approach taken. So the key to getting this right is to tackle the knowledge gap on the “state side”, to allow small teams to develop their skills and expertise in this area before taking on projects of increasing scale.
Its also clear this knowledge gap isn’t confined to the healthcare sector, but applies across the public sector (eg PULSE System in the Gardai etc is known to have related challenges), so the level of knowledge in Government of handling large IT projects needs to be tackled. Thankfully (though perhaps I need to be careful how I put this during these days of Brexit looming) the Government Digital Service team in the UK Cabinet Office, having learned the hard way with several high profile IT disasters in the public sector, has done an internationally leading job on sharing good practice in this regard and lessons can be learned from elsewhere, via their Digital Service Standard.
If you think the Digital Service Standard is some hokie-cokie public sector cook book, then take a closer look, it is very well aligned with good practice from the rest of the digital industry in terms of User Centred Design, Agile Development, Reuse of Open Source, Open Standards etc. If this good practice is happening on the ground within the Irish State sector, its hard to see it, certainly none of this level of thinking is publicly evident within the Irish public sector.
In recent years some governmental bodies world wide have neglected to build up internal capacity and capability to lead on critical Digital Service developments. In tackling digital service development (such as an Electronic Health Record) many have preferred to outsource the challenge and procure the promise of a solution from a third party vendor/supplier. The mindset is explained as “Nobody ever got fired for buying IBM“. .. what some folk crudely call the “One Throat to Choke” tactic.
So moving to a substantial procurement (e.g for an EHR) from the market in advance of building up your state side capability and capacity to handle the very complex process of procurement but especially implementation is fraught with risk in my view. Let me convey one simple reason, from past experience. During the days of the multibillion pound NHS National Programme for IT, I was witness to large groups involved in the very expensive procurement process and then some months later .. other large groups involved in the challenge of implementation of the same technology. Were these groups aligned and agreed? Certainly not.
So any large procurement (“waterfall style”) rather than user centred & iterative (“agile style”) development runs that risk. Indeed by the time the state goes to implement these technologies the folk involved in the original procurement may be long gone..
So in that vein, if , in the context of limited finances in the Irish states coffers, there is to be a shift/push for a National Childrens Hospital EHR procurement ahead of an capacity/capability building and an agile development team to prototype and understand EHR architecture, scalability, maintainability etc could be a costly mistake.
You may well ask, is there another way towards an EHR besides an expensive one off procurement? Indeed there is… again from personal experience, after leaving the travails of the NHS National IT programme, I took up a role as Chief Clinical Information Officer for Leeds Teaching Hospitals in 2009 and then Leeds City in 2012. Working with a great clinical/management and technical team (split internal/external) we developed towards the Leeds Care Record as it is today, a city wide integrated care (EHR) record system serving the professionals in primary/community/acute/mental health and social care systems to support nearly a million patients. Built on top on the internally (“state” side) developed PPM+ platform along with partner supplier (“market” side) the work involved was done in waves, with the EHR development to roll out across the city cost in the order of £2m over 3 years.. i.e. pretty good value for money. So there is another way.
The Market- which is powerful , so embed it wisely
So as we turn to the roll of the market in this challenge we repeat the words of Kate Raworth again here..
The Market: which is powerful , so embed it wisely
As we explained that the science of informatics is in its early days, so its fair to describe the health IT market is relatively immature.
The healthIT market is both dominated by a large enough number of large proprietary monoliths who promise a holistic EHR as well as by thousands of small, niche, specialist systems who offer a fragment of an EHR. The business model that most all suppliers in this market are based on depends on selling proprietary software licenses based on closed software code, rather than services oriented market based on open code.
Now if you go to look at the rest of the software market you will note that such proprietary tactics are going the way of the dinosaur… with most/many leading tech companies (even ones such as Microsoft and Apple) open sourcing their work, while other leaders such as Google and Facebook creating entire ecosystems of development based on their open source tools.
Indeed if you look beyond the vendor lockin problem in healthcare IT, to look at key issues of poor interoperability and woeful usability you will find a market that I have described as dysfunctional, ie its holding healthcare back. If you’d like to get another view, check out The Digital Doctor by US based Dr Bob Wachter;
“The Digital Doctor: Hope, Hype, Harm at the Dawn of Healthcares Computer Age” by Dr Robert Wachter, Chief Department of Medicine, UCSF, USA (2015)
“..Healthcares path to computerizations has been strewn with landmines, large and small. Medicine, our most intimately human profession, is being dehumanized by the arrival of the computer into the exam room”
“While someday the computerization of medicine will surely be that long awaited digital disruption, today it’s just plain disruptive: of the doctor patient relationship, of clinicians professional interactions’ and workflow and of the way we measure and try to improve things.”
So here we make/stress the point again, if the State cedes leadership and control of your informatics destiny by tieing itself to a proprietary EHR architecture/vendor you do so at risk.
So we need to be very careful about any major EHR procurement in 2017/18, the National Children’s Hospital being a case in point.
If you want to see the future of the EHR market, you may need to consider the future of the ERP (Enterprise Resource and Planning Market) (sidenote : PPARS was built on legacy ERP provider SAP), what Gartner have called the post modern ERP strategy.
If you’d like to understand that in a healthcare context, see this excellent article on Post Modern EHR thinking
The bottom line in terms of where the market needs to move towards and is slowly moving is that based on an open platform.
If you believe that buying an EHR system that ticks the standards box will do the trick, be very careful, you’re likely to be naieve..
Without dwelling on the details that is meant by an open platform I suggest you note this technical summary from Garnter and read more here if you want more information.
from the Gartner paper “Healthcare Provider CIOs Need to Rally Their Enterprise Architects Around Citizen-Centric Care Delivery” (2017)
“Gartner believes that truly effective and sustainable open architectures will need a capability for vendor-neutral data persistence, such as utilizing a common schema or set of archetypes and rules for managing structured and unstructured data (for example, a VNA, openEHR or IHE XDS repository in combination with services for trust/consent, ecosystem governance and oversight, and reuse of data and processes for secondary purposes, such as research and population health).
Providing open messaging standards (for example, FHIR, HL7) for data exchange in specific use cases will only go so far in meeting the architectural challenges of digital citizen-centric care delivery.”
This shift is already underway with a move to an open platform evident from Brazil to Finland to Norway to Moscow to Salford, so the key point to take aware here is that in 2017 Ireland should avoid buying into proprietary software licenses for its EHR software.
Rather than falling into the trap of being beholden to some proprietary EHR vendor for years to come, Ireland should aim break free of its economic dependence on Foreign Direct Investment by cultivating the growth of an enterprise sector aimed at supporting the leading the future direction of the healthIT market, not its past.
Is this really possible you may ask?
Well take a look at this work from 2 years ago (2015) built on this internationally leading open platform technology towards an Irish Care Record prototype.. the time involved? 1 month. the team involved? 6 people. The cost? €25,000. (If you’re a software type you’ll know exactly what can be done in 2017).
The Household which is core, so value its contribution
Having explored the pressures across the Irish healthcare system in our last post we made clear the real need to ensure the patient is much more actively involved in their own care.
Historically and currently it has been/it is too difficult for patients to navigate the healthcare system, so a paternalistic rather than cooperative and collaborative approach to healthcare delivery prevails. One of the real barriers to getting patients more involved in their healthcare is that their health and care information is scattered across the system, some in the GP record, some in the hospital record, some in the public system, some in the private system etc. etc, a painful mess with consequences..
There is therefore, very much inline with the SlainteCare push and indeed pushes long before that towards integrated care…
.. any EHR procurement in 2017 should be aimed towards building on a patient centred record platform, i.e. not simply procuring an organisation centric record such as a hospital or community EHR system, hoping to wire them up later.
Simply put, for too long healthcare systems have been stymied by siloes of information and information systems, we could/should be actively avoiding that.
Forgive me for spelling out in technical terms what that means, taking from the same recent Gartner 2017 report to make the same point from another direction.
Healthcare Provider CIOs Need to Rally Their Enterprise Architects Around Citizen-Centric Care Delivery, Gartner 2017
“Gartner believes that truly effective and sustainable open architectures will need a capability
…for managing structured and unstructured data (for example, a VNA, openEHR or IHE XDS
…providing open messaging standards (for example, FHIR, HL7) for data exchange …
will only go so far in meeting the architectural challenges of digital citizen-centric care delivery.”
So any EHR procurement effort should be going into a citizen/patient centred record effort. Am aware that some of the good folk at eHealth Ireland already get this point, they simply need to get more publicly vocal about it.
Here again its worth highlighting that a primary focus for the next 3-5 years on the National Childrens Hospital EHR rather than wider capacity/capability building around such a patient centric EHR platform across the rest of the system has real disadvantages, especially if the aim for any EHR is to support healthcare from cradle to grave..
So building on the earlier demonstration of what can be done towards an integrated Irish Care Record prototype, an early move towards a Personal Health Record on an open platform could/should be addressed at this time..
.
The Commons – which are creative, so unleash their potential
We now turn to the 4th angle on which to examine this challenge.
We have already said that the healthcare/public sector capacity/capability in large scale IT procurement is limited and needs to be addressed.
We have already highlighted the immature state of the healthIT market and the need for change.
In healthcare, for most of us educated in medicine, with the ethics and morals that go with that, many of us believe that healthcare information/knowledge should be shared between peers.
To be clear that is not to say we should improperly sharing patient information, this is simply to say that healthcare improvement will only come about at scale if we share our learning (aka “public or perish”) and our tools (e.g. it’s common to share care pathway documentation for reuse between teams etc etc)
In that spirit many of us believe that open source is the only way forward for medicine to move forward into the 21st Century.
Here we flag up the lack of a “digital commons” in Irish healthcare. What do we mean by that? Well for instance.. consider any/all of the learning that has gone into the EPR efforts in Ireland to date… is a related open place to learn and leverage from?
I might cite examples of an open digital commons such as wikipedia in the mainstream, to open access journals in healthcare, to the world of npm if you’re a software type.
Despite the presence of most of the large software suppliers in the based in Dublin, and despite the fact that many/most now support open source development ie contribute to the digital commons in healthcare.. the “digital commons”/open source scene in Ireland is fairly low profile, especially from the State side.
Some of this may be explained by inclination the the IDA towards a “knowledge development box” to encourage external companies to invest here and lock up their IP.
Now for many industries there will be no issue with that. Yet in healthcare that poses a real problem.
Let me declare here that I believe healthcare needs to be properly funded with the right level of staffing having access to the right tools at the frontline.
Let me also declare the view that healthcare monies should not be wasted again and again on poor healthIT tech with poor usability/interoperability, there has to be a better way.
So my current work, after years at the frontline in Emergency Medicine, is as a director of the non-profit Ripple Foundation, working to educate and support those people who understand this need for a digital commons in healthcare, where we work openly and collaboratively to improve healthcare with open technology.
In working towards this mission, I’m actively involved in a related 1% open digital platform push, suggesting that across the 5 Nations on these islands (Rep of Ireland, N Ireland, England, Scotland and Wales) ..and indeed beyond) that 1% of the millions of regular health IT spend could be put to better use towards this open commons goal..
Though eHealth Ireland have not actively responded on this, we know there is a real interest in this approach and a new wave of innovation on the horizon..
Thankfully this mission isn’t confined to these 5 nations either, if you look at the work of our colleagues on the recently launched Digital Square initiative based in the US and aimed across the globe, a movement has begun towards the transformation of healthcare in this century by means of openly collaborating towards a digital commons in healthcare. To explain with an excerpt from their open source mission in healthcare;
“For over a decade, PATH’s Digital Health program has been a leader in the application and use of scalable digital products and services globally and at the country level. We build on that legacy by pledging to encourage co-investment among partners and donors to support countries in seamlessly connecting their digital health systems, sharing better data, and reaching better health outcomes,” said Dr. Fleming.
As a part of this commitment, PATH is pleased to announce Digital Square. The new initiative, comprised of 40+ partner organizations, encourages more efficient investment in digital health technology solutions …. through an innovative co-investment model. “Co-investment is a simple but powerful concept. Development dollars are scarce; by coordinating them, we can maximize the impact of our financial investments,” …
It is fair to say that done right, a push towards a digital commons in Irish healthcare could not just help educate our students and professionals, transform our healthcare services, but stimulate a wave of innovation and enterprise in Ireland that would have benefit across the world too…
So its 2017, and its time to innovate our way forward in healthcare in Ireland with better healthIT.
In summary
The State which is essential- so make it accountable – needs to educate and build capacity/capability & be v careful what it procures
The Market, which is powerful , so embed it wisely – we need to move the market towards user centred digital services based on an open platform in healthcare
The Household, which is core, so value its contribution – the patient should be at the centre of healthcare – so build a patient centric platform
The Commons, which are creative, so unleash their potential – so nurture an open digital commons in healthcare to transform